Mapping disease signaling: a case study of roflumilast's potential in non-cystic fibrosis bronchiectasis

The challenge of identifying the best evidence for a well-demonstrated proof of mechanism
Multidisciplinary teams at pharmaceutical companies meticulously search through vast amounts of biomedical literature to gather evidence for underlying disease signalling mechanisms.
Conducting a robust knowledge review is time-consuming, often stretching over weeks and requiring the concerted effort of multiple experts. The resulting review tends to focus solely on articles showing direct relevance of relationships between biological entities, and overlooks a vast array of literature which may have less direct but insightful novel evidence for understanding disease signalling networks.
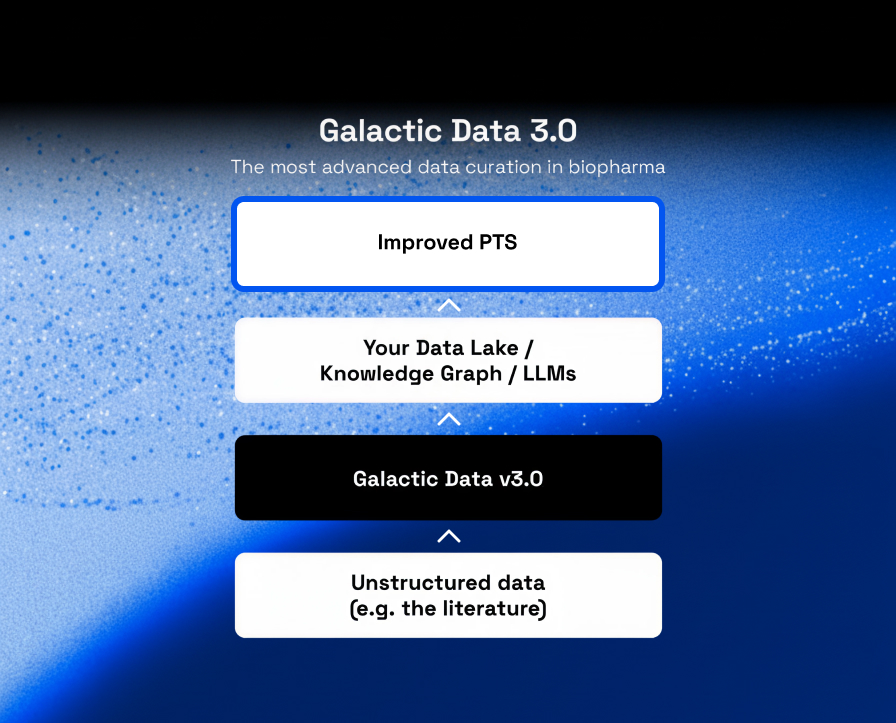
In response to these challenges, Biorelate’s unique data curation automatically identifies cause-and-effect relationships among key entities (such as drugs, genes, biological processes, and diseases). This approach is further enhanced by the latest advancements in generative artificial intelligence (generative AI), which aids in interpreting the vast quantities of data.
Exploring roflumilast's potential in non-cystic fibrosis bronchiectasis
Non-cystic fibrosis bronchiectasis represents a chronic pulmonary disorder marked by dilated bronchi, persistent neutrophilic inflammation, compromised mucus clearance, and bacterial infection1. This condition shares pathophysiological traits with chronic obstructive pulmonary disease (COPD), culminating in the progressive destruction of the airways. Roflumilast, a drug known for its efficacy in mitigating inflammation and reducing exacerbation frequency in COPD, is currently under phase II investigation for its therapeutic potential in patients with stable non-CF bronchiectasis2.
Despite its established role in COPD management, the precise mechanisms by which roflumilast quells airway inflammation in both COPD and non-CF bronchiectasis remain elusive. Roflumilast and its active derivative, roflumilast N-oxide, act as selective phosphodiesterase 4 (PDE4) inhibitors3. PDE4, a critical enzyme in the degradation of cyclic AMP within lung tissues, when inhibited, leads to an increased concentration of cyclic AMP. This elevation has been linked to significant reductions in sputum neutrophils and eosinophils, interleukin-8 (IL-8), and neutrophil elastase levels, along with a decrease in prolyl endopeptidase activity and levels of acetyl-proline-glycine-proline (AcPGP), thereby attenuating neutrophilic inflammation4.
Using Galactic AI™, Biorelate synthesised insights from various biomedical studies into a coherent mechanism that underpins roflumilast's influence on airway inflammation and its prospective clinical benefits for non-CF bronchiectasis patients, by exploring the links between roflumilast and bronchiectasis. Request the full case study here.
Our analysis facilitates the extraction of pivotal cause-and-effect relationships, validating clinical observations to date and shedding light on roflumilast's influence on bronchiectasis signalling mechanism:
- Roflumilast's PDE4 inhibition modulates inflammatory pathways within the airways, potentially reducing exacerbations in bronchiectasis.
- The significant roles of CXCL8 (IL-8) and ELANE (neutrophil elastase) in bronchiectasis underscore a logical mechanism for roflumilast's therapeutic action.
Furthermore, our findings suggest additional pathways through which roflumilast may exert its effects:
- A detailed mechanistic link connecting roflumilast, PDE4, CXCL8, ELANE, and the inflammatory response.
- Novel hypotheses on roflumilast's potential to modulate mucus secretion via its impact on TNF-alpha and CFTR.
- The identification of intermediary cytokines as potential pharmacodynamic biomarkers for validating the proposed mechanisms.
Request the full case study PDF report to get the full story of our approach and findings.
By synthesising and summarising directed pathways of cause-and-effect from millions of articles, Biorelate's method offers a streamlined process for exploring the mechanism of action between drugs, drug targets and diseases. You can see the full case study of examples of this approach by requesting the PDF.
References
- Choi, J. Y. Exacerbation Prevention and Management of Bronchiectasis. Tuberc Respir Dis 86, 183–195 (2023).
- Study Details | Roflumilast in Non-CF Bronchiectasis Study (2019) | ClinicalTrials.gov. https://www.clinicaltrials.gov/study/NCT04322929
- Zhang, X. et al. Pharmacological mechanism of roflumilast in the treatment of asthma-COPD overlap. Drug Des Devel Ther 12–2371 (2018) doi:10.2147/DDDT.S165161.
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/022522s000lbl.pdf
Latest News
Discover new insights and updates for data science in biopharma